Interoperability – all that’s old is new again
Interoperability – all that’s old is new again
For some of us in health care policy, 2018 so far is the year of testing just how good our filing systems are. All that is old is new again and ideas to “fix the U.S. health care system” from years ago are popping back up. This week “interoperability” is the hot topic, in part because Seema Verma, Administrator of the Centers for Medicare & Medicaid Services (CMS), made a big announcement at the Healthcare Information and Management Systems Society (HIMSS) annual conference, saying interoperability would again be a focus of the federal government. She made three big announcements really, but today we are focused on Verma’s announcement that CMS will be overhauling the “Electronic Health Record (EHR) Incentive Programs to refocus the programs on interoperability and to reduce the time and cost required of providers to comply with the programs’ requirements.” Not surprisingly, when she mentioned the burdens on health providers of meeting meaningful use requirements and that CMS would be changing those requirements, the full ballroom broke into applause.
Patients Should Control Their Data. Yes, but…
The CMS administrator also announced a new initiative, “MyHealthEData – to empower patients by giving them control of their healthcare data, and allowing it to follow them through their healthcare journey.” It may seem obvious that patients should have electronic access to, and full control of, their health records, but the government does seem to need to intervene in order to get this information released from government agencies and payers, as well as from private health insurers and providers. Susan Morse (@SusanJMorse), who covered the HIMSS Conference for Healthcare IT News, explains that part of the issue is hospitals involved in data blocking. Verma told conference goers CMS would be strengthening requirements for providers to stop the practice: “It’s not acceptable to limit patient records or prevent them from seeing their complete history outside of (that) health system,” she said.
Data blocking may not be the primary barrier to patient control of their health care data, however. The March 2018 American Hospital Association Trendwatch: Sharing Health Information for Treatment shows hospitals and health systems have rapidly improved electronic sharing of clinical/summary care records over the past several years as the AHA Trendwatch chart below shows.
Can (Will?) Health Providers Use Patient Data?
Interoperability at its core means information can move back and forth between the various entities that have it. That could be from provider to provider, from plan to provider, provider to patient, etc. The fact sheet explaining the Trump Administration MyHealthEData Initiative Putting Patients at the Center of the U.S. Healthcare System mentions one of the goals of the effort is:
“Reducing Duplicative Testing – Provider systems typically do not share patients’ data, which can lead to duplicative tests when a patient goes to see a different provider. This increases costs and can lead to patient inconvenience or even harm. CMS is studying the extent and impact of duplicate testing, and will identify ways to reduce the incidence of unnecessary duplicate testing.”
In a study published in 2010, (all that’s old is new again…) in the Journal of the American Medical Informatics Association titled, “A Preliminary Look at Duplicate Testing Associated With Lack of Electronic Health Record Interoperability For Transferred Patients,” found approximately 20% of patients had non-clinically indicated duplicate testing resulting in added costs to the system. The study authors continued, “The most common setting for duplicate testing identified in the current study happened on admission from an outpatient clinic site. Patients from outpatient clinic transfer to hospital admission via several paths, including entrance via hospital admitting services or directly to the inpatient ward, either escorted or unescorted by hospital clinical staff.”
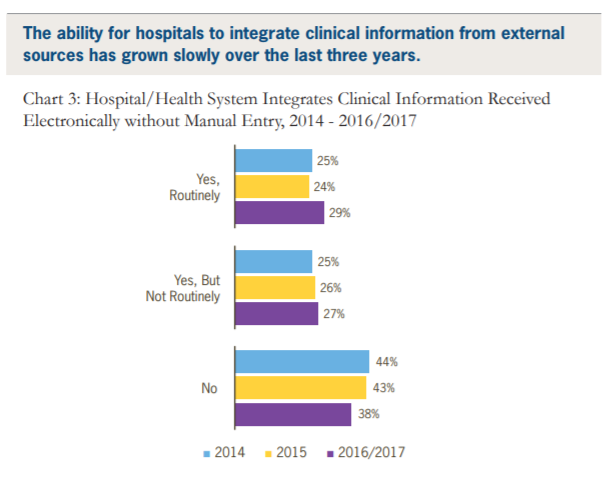
However, while hospitals and health systems have improved their sharing of clinical summaries with outside entities, the same AHA Trendwatch shows much slower progress in integrating information from outside sources. As the chart (from AHA Trendwatch) below shows, 65% of hospitals and health systems are either not able or not routinely able to integrate external information electronically.
Giving patients access to all of their health care data electronically is no doubt important. However, it is not sufficient to improve care or reduce costs, even for something as simple as avoiding non-clinically indicated duplicate testing. Achieving interoperability will also require payment incentives to change. As this blog has pointed out in other instances, money matters and you avoid what you have to pay for. Electronic health data vendors can still charge providers for building interfaces that help disparate systems “talk” and can charge providers to move data. Keith Aldinger, MD, an internist who practices in Houston, Texas wrote for Medical Economics in late 2017, physicians have “been assessed financial penalties for not attesting to meaningful use and yet the IT industry gets a pass.” His idea for improving interoperability is to put health IT vendors on the hook: “They should not be allowed to charge one cent for transferring information and any attempt to do so should elicit a financial penalty.”
All that’s old is new again. We still have to figure out how to get health care data moving in ways that improve health care for patients. Interoperability, you’re hot again. Let’s hope you do better this time around.